Cyclone Fanatics –
Today we’re going to learn about meniscus tears and how they are treated by orthopedic surgeons. The ‘take home message’ here is: SAVE the MENISCUS (if possible).
First off, let me give you a typical scenario: A high school athlete twists a knee and tears a meniscus. The knee is scoped and the meniscus tear is trimmed out. Recovery is straightforward and the athlete gets back quickly. Everything goes well for about 15 years when they start to get a little ache in the knee with activity. This gradually worsens over time and then they see an orthopedic surgeon who gets x-rays and tells them they are starting to get some arthritis.
This can progress over the next 10 years or so, sometimes leading to the need for a knee replacement. What is that all about? How can a knee scope as a teenager sometimes lead to a knee replacement in your 50s? Before we answer that question, let’s do some anatomy review.
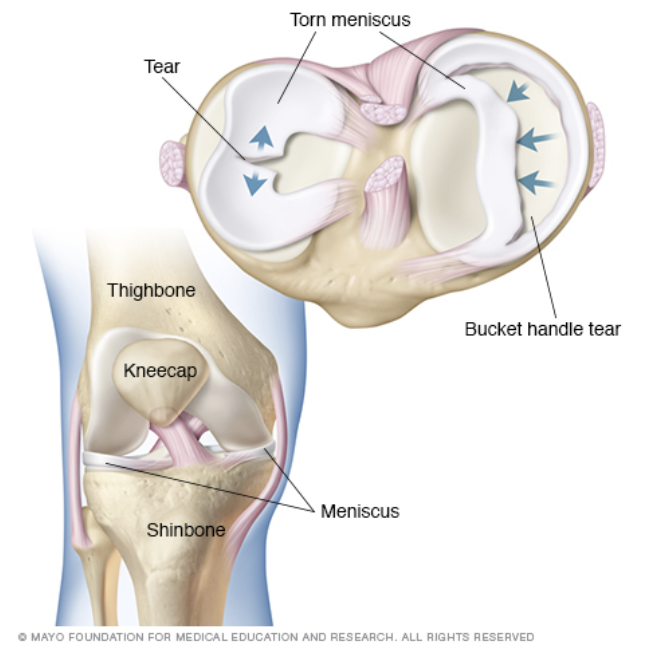
The meniscus is the cartilage in the knee that functions as the ‘shock-absorber’ for the knee.
It can be injured and torn by any type of sudden twisting motion, leading to symptoms of popping, clicking, catching and swelling, with associated pain. This is typically treated by an orthopedic surgeon using arthroscopy, an outpatient surgery where tiny incisions are made to enter the knee joint, using fiber optics for visualization, with the torn fragment being removed. Every year there are well over a million knee arthroscopies performed in the US, with over half of these being performed to treat meniscal tears.
An intact meniscus is important over the long-term in providing health for the knee joint, and injury to the meniscus necessitating (even partial) removal of the meniscus can lead to arthritis in the knee. Risk factors for this would be increased weight, family history of knee arthritis and getting more meniscus removed. In laymen’s terms, the loss of the meniscus alters the forces across the joint and, over time, this can lead to increased ‘wear and tear’ arthritis.
That’s why it is PARAMOUNT to try and SAVE the MENISCUS, if possible. Your orthopedic sports medicine surgeon should be experienced with the ability to repair the meniscus, if that is possible and reasonable. (Note–some tears are a pattern that can’t technically be repaired, and some tears are so”beat up” that it doesn’t even make sense to try a repair). I especially try and do MENISCAL REPAIRS if associated with ACL reconstruction. This repair situation has a higher rate of healing, and doesn’t change the overall ACL rehab.
I prefer the ALL-INSIDE technique of repair, and have had good success with the AIR system. Check out this video demonstrating a meniscal repair.
Meniscus transplant (transferring a cadaver meniscus into a patient’s knee) has been a possibility for those without a meniscus (and having no accompanying arthritis) but there are some clinical limitations.
A newer development is the Collagen Meniscus Implant (CMI®). This is a FDA-approved meniscus implant, utilizing the all-inside repair system, which is biological and completely absorbable. The highly purified collagen is a porous structure that is arthroscopically attached to fill the void resulting from damaged/lost meniscal tissue and then makes use of the body’s own healing ability. Basically the CMI serves as a guide for the migration of the body’s own cells and then is completely absorbed afterwards, leaving behind a “new meniscus.”
This new and biomechanically competent meniscus-like tissue forms by supporting new tissue ingrowth. Studies show that the tissue is safe (it’s the patient’s own body healing itself) and appears to enhance meniscal function as evidenced by improved clinical outcomes in patients with a chronic meniscal injury.
Thus CMI has the possibility to be used in some patients to replace irreparable or lost meniscal tissue in patients with a chronic (not acute) injury. (For more info check out.)
CMI use requires certification so check with your orthopedic sports medicine specialist to see if you might be a candidate. And don’t hesitate to call McFarland Clinic Orthopedic Sports Medicine if you have further questions about CMI, or about knee arthroscopy and the goal to SAVE the MENISCUS (if possible)!!!
Call 515-239-4475, and ask for the surgeons who take care of the Cyclones; Drs. Greenwald, Warme and Buck.
Let’s hope for another great road win for Matt Campbell’s boys, as they head to West Virginia. And, as always, Go Cyclones!
Thomas Greenwald, MD